Publication
Article
Pharmacy Times
Pertussis: A Preventable Paroxysmal Cough
Author(s):
Before a pertussis vaccine was widely available, about 200,000 American children contracted this highly contagious acute respiratory tract infection annually, and between 4000 and 9000 children died each year.
Consider this: Before a pertussis vaccine was widely available, about 200,000 American children contracted this highly contagious acute respiratory tract infection annually, and between 4000 and 9000 children died each year.1,2 Vaccines were developed in 1914 and refined in the 1940s. By 2004, successful campaigns had reduced the number of reported pertussis cases to fewer than 16,000 and the number of deaths to just 27.2 Immunization prevents this bacterial infection caused by Bordetella pertussis, yet the nation saw a 2300% increase in cases between 1976 and 2005.3 What is the problem?
Also called whooping cough for its characteristic paroxysmal cough, pertussis is especially dangerous for children younger than 2 years. Children are not fully immune until they receive at least 3 shots in the recommended series, and the vaccine’s protection typically falls 3 to 5 years after vaccination. After 12 years, immunity is gone.4-6
Before a vaccine was developed, pertussis was mainly a childhood disease. Today, pertussis affects primarily infants and toddlers who have not been completely immunized (see Table 17,9-11) and teenagers and adults whose immunity has waned. Although treatable with antibiotics, usually macrolides, pertussis can also be serious for youths and adults.7
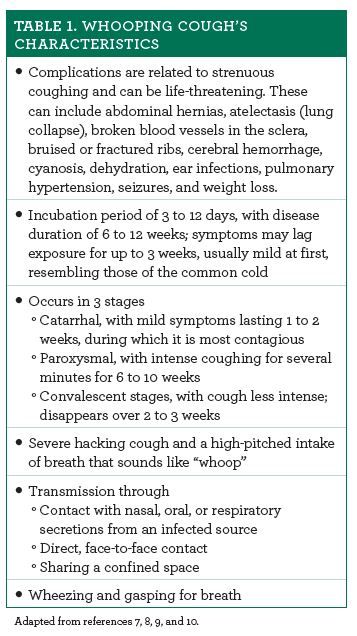
What Is Whooping Cough?
When infected individuals cough or sneeze, they spray microbe-laden droplets into the air. Inhaled by others, bacteria produce a toxin that severely damages the lungs’ cilia and respiratory epithelium. The subsequent difficulty clearing pollen, mucus, and microbial invaders causes uncontrollable coughing.8
The vaccine does not provide lifelong immunity. Pregnant women and all others who have close contact with an infant are potential disease reservoirs.8
This explains recent increases in pertussis cases. People of all age groups have been affected, but the highest annual incidence is in infants younger than 1 year.12 Death is most likely in infants younger than 3 months.12 Historically, mothers have been most likely to transmit pertussis to their infants, but now siblings have taken on that dubious honor.10,13 Those statistics reveal risk factors in addition to infancy. These are contact with individuals whose vaccine-induced immunity has waned, contact with unimmunized people, and living with an infected person in the same household.10,13 Premature infants and patients with underlying cardiac, neurologic, neuromuscular, pulmonary, or respiratory disease are also at risk.10,13
The Pharmacist’s Role
Pharmacists’ primary roles in pertussis are preventive. Pertussis spreads quickly, and waning vaccination-induced immunity means that we cannot depend on everlasting herd immunity to protect everyone.14 Individuals at risk for exposure or with close contact with an infant need booster shots at or after age 11 and then every 10 years and during pregnancy.15,16 Asking about pertussis immunization and providing basic information to patients can prompt vaccination.
If an individual appears to have whooping cough, pharmacists should refer the patient to a prescriber immediately, especially if the patient is an infant. Severe symptoms are red flags that the patient needs emergency urgent care. Consider sending a list of all medications, dates and names of previous immunizations, medication allergies, and past medical conditions with the patient if possible.
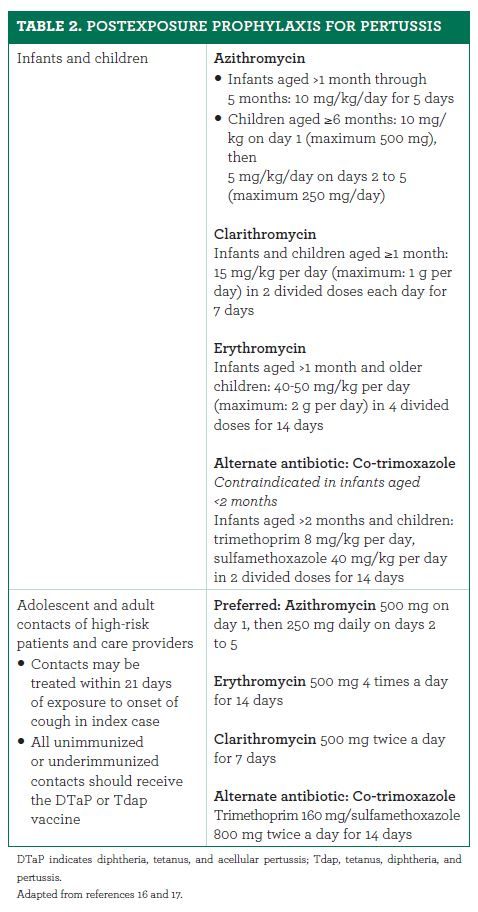
Pharmacists should also be aware of postexposure prophylaxis recommendations (see Table 216,17), especially for families who choose not to vaccinate.
Jeannette Y. Wick, RPh, MBA, FASCP, is the assistant director of the Office of Pharmacy Professional Development at the University of Connecticut School of Pharmacy in Storrs.
References
- Before the age of vaccination. Pittsburgh-Post Gazette. October 31, 2000. old.post-gazette.com/healthscience/20001031hvaccines.asp. Accessed February 25, 2018.
- Roush SW, Murphy TV; Vaccine-Preventable Disease Table Working Group. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298(18):2155-2163. doi: 10.1001/jama.298.18.2155.
- Centers for Disease Control and Prevention. Outbreaks of respiratory illness mistakenly attributed to pertussis—New Hampshire, Massachusetts, and Tennessee, 2004-2006. MMWR Morb Mortal Wkly Rep. 2007;56(33):837-842.
- Centers for Disease Control and Prevention. Notes from the field: use of tetanus, diphtheria, and pertussis vaccine (Tdap) in an emergency department - Arizona, 2009-2010. MMWR Morb Mortal Wkly Rep. 2012;61(3):55-56.
- Winter K, Harriman K, Zipprich J, et al. California pertussis epidemic, 2010. J Pediatr. 2012;161(6):1091-1096. doi: 10.1016/j.jpeds.2012.05.041.
- Centers for Disease Control and Prevention. Pertussis epidemic - Washington, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(28):517-522.
- Cornia PB, Hersh AL, Lipsky BA, Newman TB, Gonzales R. Does this coughing adolescent or adult patient have pertussis? JAMA. 2010;304(8):890-896. doi: 10.1001/jama.2010.1181.
- Walsh PF, Kimmel L, Feola M, et al. Prevalence of Bordetella pertussis and Bordetella parapertussis in infants presenting to the emergency department with bronchiolitis. J Emerg Med. 2011;40(3):256-261. doi: 10.1016/j.jemermed.2008.04.048.
- Bisgard KM, Pascual FB, Ehresmann KR, et al. Infant pertussis: who was the source? Pediatr Infect Dis J. 2004;23(11):985-989.
- Skoff TH, Kenyon C, Cocoros N, et al. Sources of infant pertussis infection in the United States. Pediatrics. 2015;136(4):635-641. doi: 10.1542/peds.2015-1120.
- Centers for Disease Control and Prevention. Pertussis - United States, 2001-2003. MMWR Morb Mortal Wkly Rep. 2005;54(50):1283-1286.
- Committee opinion no. 718 summary: update on immunization and pregnancy: tetanus, diphtheria, and pertussis vaccination. Obstet Gynecol. 2017;130(3):668-669. doi: 10.1097/AOG.0000000000002293.
- Kline JM, Lewis WD, Smith EA, et al. Pertussis: a reemerging infection. Am Fam Physician. 2013;88(8):507-514.
- McGirr A, Fisman DN. Duration of pertussis immunity after DTaP immunization: a meta-analysis. Pediatrics. 2015;135(2):331-343. doi: 10.1542/peds.2014-1729.
- Dajani N, Scheifele D. How long can we expect pertussis protection to last after the adolescent booster dose of tetanus-diphtheria-pertussis (Tdap) vaccines? Pediatr Child Health. 2007;12(10):873-874.
- About pertussis outbreaks. Centers for Disease Control and Prevention website. cdc.gov/pertussis/outbreaks/about.html. Updated August 7, 2017. Accessed February 25, 2018.
- Woo TM. Postexposure management of vaccine-preventable diseases. J Pediatr Health Care. 2016;30(2):173-182. doi: 10.1016/j.pedhc.2015.12.006.